By: Dr. Rami Rustum – July, 2016
Fibromyalgia is a chronic disorder marked by widespread, unexplained pain in the muscles and joints. It’s not a disease. It’s a syndrome, which is a collection of symptoms that occur together. Although many people think of it as an arthritic condition due to the symptoms, it’s not a type of arthritis.
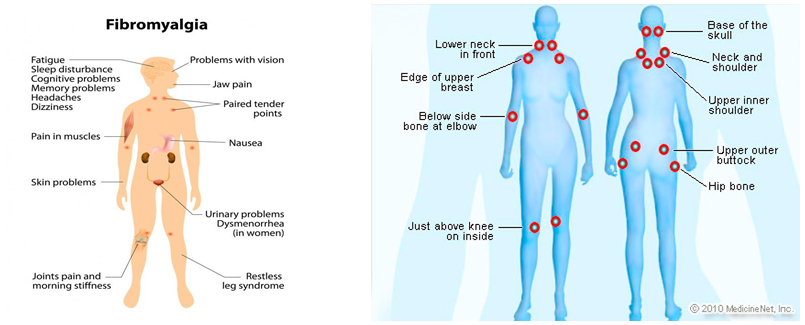
The condition is often associated with tender points, which are termed “trigger points.” These are places on the body where even light pressure causes pain. According to standards published by the American College of Rheumatology in 1990, a person can be diagnosed with fibromyalgia if they have widespread pain and tenderness in at least 11 of the known 18 trigger points. Newer guidelines don’t require a tender point exam. Instead, a fibromyalgia diagnosis can be made if a person has had widespread pain for more than three months with no underlying medical condition that could cause the pain.
Common trigger points include:
• the back of the head
• tops of shoulders
• upper chest
• hips
• knees
• outer elbows
A consistent dull ache through the entire body is also common. People with this disorder may also have: fatigue, trouble sleeping, headaches, depression and anxiety.
Although the causes are unclear, fibromyalgia flare-ups can be the result of stress, physical trauma, or an apparently unrelated systemic illness like the flu. Symptoms may be a result of the brain and nerves misinterpreting or overreacting to normal pain signals. This could be possibly due to an imbalance in brain chemicals.
Doctors don’t know what causes fibromyalgia which may affect up to 5 million patients every year, but it most likely involves a variety of factors working together. These may include:
• Genetics. Because fibromyalgia tends to run in families, there may be certain genetic mutations that may make you more susceptible to developing the disorder.
• Infections. Some illnesses appear to trigger or aggravate fibromyalgia.
• Physical or emotional trauma. Post-traumatic stress disorder has been linked to fibromyalgia.
Risk factors for fibromyalgia include:
• Your sex. Fibromyalgia is diagnosed more often in women than in men.
• Family history. You may be more likely to develop fibromyalgia if a relative also has the condition.
• Rheumatic disease. If you have a rheumatic disease, such as rheumatoid arthritis or lupus, you may be more likely to develop fibromyalgia.
The pain and lack of sleep associated with fibromyalgia can interfere with your ability to function at home or on the job. The frustration of dealing with an often-misunderstood condition also can result in depression and health-related anxiety.
While there is no lab test to confirm a diagnosis of fibromyalgia, your doctor may want to rule out other conditions that may have similar symptoms. Blood tests may include:
• Complete blood count
• Erythrocyte sedimentation rate
• Thyroid function tests
Treatment: There is no cure for fibromyalgia. However, symptoms can be treated with both medication and non-drug treatments. Many times the best outcomes are achieved by using multiple types of treatments. Medications: The U.S. Food and Drug Administration has approved three drugs for the treatment of fibromyalgia. They include two drugs that change some of the brain chemicals that help control pain levels: duloxetine (Cymbalta) and milnacipran (Savella). Older drugs that affect these same brain chemicals also may be used to treat fibromyalgia. These include amitriptyline (Elavil) and cyclobenzaprine (Flexeril). Other antidepressant drugs can be helpful in some patients. Side effects vary by the drug. The other drug approved for fibromyalgia is pregabalin (Lyrica). Pregabalin and another drug, gabapentin (Neurontin), work by blocking the over activity of nerve cells involved in pain transmission. These medicines may cause dizziness, sleepiness, swelling and weight gain.
It is NOT recommended opioid narcotics for treating fibromyalgia. The reason for this is that research evidence suggests these drugs are not of great benefit to most people with fibromyalgia. In fact, they may cause greater pain sensitivity or make pain persist. Tramadol (Ultram) may be used to treat fibromyalgia pain if short-term use of an opioid narcotic is needed. Over-the-counter medicines such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (commonly called NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve) are not effective for fibromyalgia pain. Yet, these drugs may be useful to treat the pain triggers of fibromyalgia. Thus, they are most useful in people who have other causes for pain such as arthritis in addition to fibromyalgia.
For sleep problems, some of the medicines that treat pain also improve sleep. These include cyclobenzaprine (Flexeril), amitriptyline (Elavil), gabapentin (Neurontin) or pregabalin (Lyrica). It is not recommended that patients with fibromyalgia take sleeping medicines like zolpidem (Ambien) or benzodiazepine medications. Other Therapies: People with fibromyalgia should use non-drug treatments as well as any medicines their doctors suggest. Research shows that the most effective treatment for fibromyalgia is physical exercise. Physical exercise should be used in addition to any drug treatment. Patients benefit most from aerobic exercises. Cognitive behavioral therapy is a type of therapy focused on understanding how thoughts and behaviors affect pain and other symptoms. Other complementary and alternative therapies such as acupuncture, chiropractic and massage therapy, can be useful to manage fibromyalgia symptoms. Many of these treatments, though, have not been well tested in patients with fibromyalgia.
|
|